21-ways-triggering-appointmt copy
Candice Pert, Molecule of Emotion
Anthony DeMasio; The Feeling of What Happens (brain development) (NY Times web site)
Brennan, Barbara, (1993). Book Light Emerging. Bantam Book.
Kurtz, Ron (1990) Book. Hakomi Method Body-Centered Psychotherapy. Life Rhythm; Mendocino, CA.
Levine, Peter, (1997). Book Waking the Tiger. Berkeley, CA: North Atlantic Books.
Rand, Marjorie; Rosenberg, Jack Lee (1991). Book. Body Self, and Soul. Humanics New Age, Atlanta, Georgia.
Rosenberg, Jack, Kitaen-Morse, Beverly (1996). Book. The Intimate Couple. Turner Publishing, Inc.; Atlanta, GA.
Rothschild, Babette (2000). Book. The Body Remembers. W.W. Norton & Company, New York, London.
The Lasting Effects of Psychological Trauma on Memory and the Hippocampus
J. Douglas Bremner, M.D.
Departments of Diagnostic Radiology and Psychiatry,
Yale University School of Medicine, Yale Psychiatric Institute,
and National Center for PTSD-VA Connecticut Healthcare System
Dr. Bremner reports no commercial conflict of interest.
This research reviewed in this paper was supported by a NIH-sponsored General Clinical Research Center (GCRC) Clinical Associate Physician (CAP) Award and a VA Research Career Development Award to Dr. Bremner, and the National Center for PTSD Grant.
Educational Objectives
Upon completion of this Cyberounds®, the participant should be able to:
- Discuss how extreme stressors, including childhood abuse and combat, can have lasting effects on hippocampal-based verbal declarative memory and what the relevance of this to education, public policy, rehabilitation and psychiatric treatment
- Describe research findings showing reduction in volume of the hippocampus in posttraumatic stress disorder related to abuse or combat andtheoretical explanations for findings
- Describe how dysfunction of medial prefrontal cortex may contribute to symptoms of stress-related disorders like PTSD.
The invisible epidemic
The invisible epidemic of childhood abuse and other psychological traumas and stressors represents a major public health problem in our society today. Childhood sexual abuse alone affects 16% of women (about 40 million) in the U.S.A. (including rape, attempted rape, or molestation) at some time before their 18th birthday.1
Childhood abuse is the most common cause of posttraumatic stress disorder (PTSD) in women, which affects 8% of the population at some time in their lives,2 although there are a range of other types of psychological trauma that can also lead to symptoms of chronic PTSD, including car accidents, combat, rape and assault. Some of the symptoms of PTSD, which include intrusive memories, nightmares, flashbacks, increased startle and vigilance, social impairment and problems with memory and concentration, may be related to the effects of extreme stress on the brain.3,4
Individuals with a history of exposure to childhood abuse or combat had a reduction in volume of a brain area involved in learning and memory called the hippocampus, which is felt to be related to stress, with associated deficits in hippocampal-based learning and memory.5 Children under stress develop impairments in academic achievement that are specifically related to the development of PTSD. Other symptoms, including fragmentation of memory, intrusive memories, flashbacks, dissociation and pathological emotions, may also be related to hippocampal dysfunction6 and may explain delayed recall of childhood abuse.7 The hippocampus has important links to the medial prefrontal cortex, another brain area that mediates emotion and the stress response, dysfunction of which has also been implicated in PTSD.
A disease of memory
Alterations in memory form an important part of the clinical presentation of patients with PTSD. PTSD patients report deficits in declarative memory (remembering facts or lists, as reviewed below), fragmentation of memories (both autobiographical and trauma-related) and dissociative amnesia (gaps in memory that can occur for minutes to days and are not due to ordinary forgetting).
Psychiatric Symptoms Associated with Childhood Abuse
PTSD
- Nightmares
- Flashbacks
- Memory & Concentration problems
- Hyperarousal
- Hypervigilance
- Intrusive memories
- Avoidance
- Startle reponses
- Feeling worse with traumatic reminders
Dissociative
- Out of body experiences
- Derealization
- Amnesia
- Fragmented sense of self & identity
Anxiety
- Panic attacks
- Claustrophobia
Substance Abuse
- Alcoholism
- Opiate addiction
Many abuse victims claim to remember only certain aspects of the abuse event. For instance, a patient who was locked in the closet had an isolated memory of the smell of old clothes and the sound of a clock ticking. Later, she connected that with feelings of intense fear and, then, the entire circumstances relating to the abusive events. PTSD is also associated with alterations in non-declarative memory (i.e., types of memory that cannot be willfully brought up into the conscious mind, including motor memory, such as how to ride a bicycle). These types of non-declarative memories include conditioned responses and abnormal reliving of traumatic memories following exposure to situationally appropriate cues. Many of these memory disturbances may be related to dysfunction of the hippocampus and related brain areas such as medial prefrontal cortex.
Effects of psychological trauma on the hippocampus and memory
Childhood abuse and other extreme stressors can have lasting effects on brain areas involved in memory and emotion. The hippocampus is a brain area involved in learning and memory that is particularly sensitive to stress.8,9 As reviewed in greater detail by Bruce McEwen in other Cyberounds high levels of glucocorticoids (cortisol in the human) released during stress were associated with damage to neurons in the CA3 region of the hippocampus, and a loss of neurons and dendritic branching.10,11,12 Glucocorticoids disrupt cellular metabolism and increase the vulnerability of hippocampal neurons to excitatory amino acids like glutamate.13 Other neurochemical systems interact with glucocorticoids to mediate the effects of stress on memory and the hippocampus, including serotonin14 and brain-derived neurotrophic factor (BDNF).15,16 Stress also results in deficits in new learning that are secondary to damage to the hippocampus.17,18 Exciting recent research has shown that the hippocampus has the capacity to regenerate neurons and that stress inhibits neurogenesis in the hippocampus.19
Studies in animals showing glucocorticoid-mediated hippocampal toxicity and memory dysfunction with stress raised the question: Does early stress, such as childhood abuse, result in similar deficits in human subjects? With this in mind, we used neuropsychological testing to measure declarative memory function in PTSD. We selected measures that were validated in studies of patients with epilepsy to be specific probes of hippocampal function. These neuropsychological measures (including delayed paragraph recall and word list learning) were correlated with a loss of neurons in the hippocampus in patients who underwent surgical resection of the hippocampus for the treatment of epilepsy.20 We initially found verbal declarative memory deficits using similar measures in Vietnam combat veterans with PTSD.21
In the first report to use brain imaging in PTSD, combat veterans were found to have an 8% reduction in right hippocampal volume, measured with magnetic resonance imaging (MRI), with no difference in comparison regions including caudate, amygdala and temporal lobe (Figure 1).
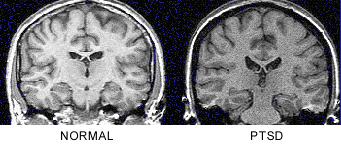
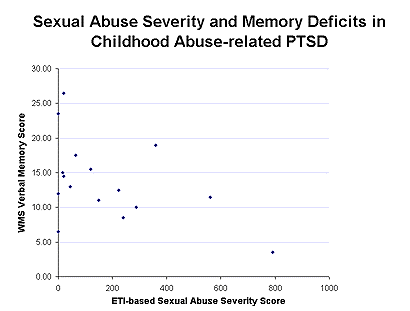
Decreases in right hippocampal volume in the PTSD patients were associated with deficits in short-term memory (r=0.64; p<0.05).22 This initial report was replicated in survivors of childhood physical and/or sexual abuse with PTSD. We found similar deficits in short-term memory as in the combat veterans, which were correlated with level of abuse as quantitated with the Early Trauma Inventory23 (Figure 2) and a 12% reduction in left hippocampal volume.24
Two other replications of the original study have now been reported showing hippocampal volume reduction in PTSD.25,26 Our preliminary data show a failure of hippocampal activation measured with PET during memory retrieval in PTSD. We also showed that hippocampal volume reduction is specific to PTSD and not other anxiety disorders (panic disorder).
Studies are ongoing to assess the effects of treatments on hippocampal volume in PTSD using medications, including fluoxetine and phenytoin, that were shown in animal studies to increase dendritic branching or block the effects of stress on the hippocampus. We are also comparing monozygotic twins with and without PTSD to rule out the possibility that smaller hippocampal volume at birth can explain findings of hippocampal volume reduction in PTSD, acting as a type of risk factor.
The hippocampus has an inhibitory effect release of corticotropin releasing factor (CRF) from the pituitary. CRF plays a critical role in the stress response, both mediating peripheral HPA axis activation in stress and acting centrally to mediate fear-related behaviors and chronic stress in animals was shown to lead to chronic increases in CRF release. Again consistent with hippocampal dysfunction, we found elevations of concentrations of CRF in the cerebrospinal fluid (CSF) in PTSD.27
Empirical studies on memory and the hippocampus may shed some light on the controversy surrounding delayed recall of memories of childhood abuse. The hippocampus plays an important role in integrating or binding together different aspects of a memory at the time of recollection and is felt to be responsible for locating the memory of an event in time, place and context. We have hypothesized that atrophy and dysfunction of the hippocampus, following exposure to childhood abuse, may lead to distortion and fragmentation of memories.7 For instance, in an abused patient who was locked in the closet, there is a memory of the smell of old clothes but no visual memory of being in the closet and no affective memory of the feeling of fear. Perhaps, with psychotherapy, there is a facilitation of associations to related events that may bring all of the aspects of the memory together. Or, if the patient has an event such as being trapped in a dark elevator, the feeling of fear with darkness and the enclosed space may be enough to trigger a recollection of the entire memory.
The effects of childhood trauma on memory and the brain also have important implications for public health policy. This is especially pertinent for inner-city children who often witness violent crimes in their neighborhoods and families, in addition to trauma, such as childhood abuse. If abused children have damage to brain areas involved in learning and memory, this may put them at a serious disadvantage that programs such as Head Start will not be able to overcome. Consistent with this, traumatized Beirut adolescents with PTSD had deficits in academic achievement, compared to non-traumatized adolescents and traumatized adolescents without PTSD.28
Dysfunction of the medial prefrontal cortex in PTSD
Abnormalities of other brain areas (Figure 3), including medial prefrontal cortex, are also associated with PTSD.
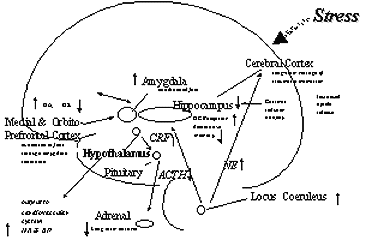
Medial prefrontal cortical areas modulate emotional responsiveness and mediate conditioned fear responses to fear-inducing stimuli through inhibition of amygdala function.29 We have hypothesized that dysfunction in these regions may underlie pathological emotional responses in patients with PTSD.30 This area also has important functional connections with the hippocampus. In several studies using positron emission tomography (PET) imaging of brain function in PTSD, we have found dysfunction of the medial prefrontal cortex and hippocampus during provocation of PTSD symptoms and presentation of traumatic cues. We stimulated PTSD symptoms with the noradrenergic agent, yohimbine. We found a relative failure of activation in metabolism in parts of medial prefrontal cortex (orbitofrontal), decreased function in hippocampus, in comparison to placebo and in comparison to responses in healthy subjects.31
In a study using combat-related slides and sounds to provoke PTSD symptoms, combat veterans with PTSD (but not combat veterans without PTSD) demonstrated a decrease in blood flow in the medial prefrontal cortex (Brodmann’s area 25 or subcallosal gyrus) (Figure 4), with a failure of activation in anterior cingulate (area 32 and 24) and increased activation in posterior cingulate, motor cortex and lingual gyrus.32
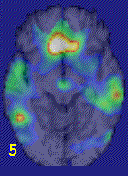
Women with childhood sexual abuse and PTSD, compared to sexually abused women without PTSD, exposed to personalized scripts of childhood sexual abuse, again showed decreased blood flow in medial prefrontal cortex (area 25) and failure of activation in anterior cingulate, with increased blood flow in posterior cingulate and motor cortex. PTSD women also had decreased blood flow in right hippocampus. These imaging findings are consistent with dysfunction of medial prefrontal cortex and hippocampus in PTSD that may underlie pathological emotions in these patients.
Summary
This review has covered the broad impact of childhood abuse and other traumas on memory and the hippocampus. The hippocampus, a brain area involved in verbal declarative memory, is particularly sensitive to stress. Patients with combat and abuse-related PTSD were shown to have smaller hippocampal volume and deficits in hippocampal-based verbal declarative memory functions. Hippocampal dysfunction may underlie many symptoms of PTSD and may explain elevations in concentrations of CRF in PTSD. Another brain area affected by stress is the medial prefrontal cortex. Functional imaging studies show dysfunction in this area (as well as hippocampus) during provocation of PTSD symptoms and presentation of traumatic reminders. Medial prefrontal cortical inhibition of amygdala responsiveness is felt to underlie extinction to fear responding. Dysfunction of this area in abuse-related PTSD may lead to problems modulating emotion in PTSD.

References
1. McCauley J, Kern DE, Kolodner K, Dill L, Schroeder AF, DeChant HK, Ryden J, Derogatis LR, Bass EG (1997). Clinical characteristics of women with a history of childhood abuse: Unhealed wounds. JAMA 277:1362-1368. return
2. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB (1995). Posttraumatic stress disorder in the national comorbidity survey. Arch Gen Psychiatry 52:1048-1060. return
3. Bremner JD, Marmar C (eds.) (1998): Trauma, Memory and Dissociation, APA Press, Washington DC. return
4. Saigh PA, Bremner JD (Eds.) (1999). Posttraumatic Stress Disorder: A Comprehensive Text, Allyn & Bacon, New York. return
5. Bremner JD, Narayan M (1998): The effects of stress on memory and the hippocampus throughout the life cycle: Implications for childhood development and aging. Develop Psychopath 10:871-886. return
6. Bremner JD, Southwick SM, Charney DS (1999): The neurobiology of posttraumatic stress disorder: An integration of animal and human research. In: Saigh, P., Bremner, J.D. (Eds.): Posttraumatic Stress Disorder: A Comprehensive Text, Allyn & Bacon, New York, pp. 103-143. return
7. Bremner JD, Krystal JH, Charney DS, Southwick SM (1996): Neural mechanisms in dissociative amnesia for childhood abuse: Relevance to the current controversy surrounding the "False Memory Syndrome". Am J Psychiatry 153(7):FS71-82. return
8. McEwen BS, Angulo J, Cameron H, Chao HM, Daniels D, Gannon MN, Gould E, Mendelson S, Sakai R, Spencer R, Woolley C (1992): Paradoxical effects of adrenal steroids on the brain: Protection versus degeneration. Biol Psychiatry 31:177-199. return
9. Sapolsky RM (1996). Why stress is bad for your brain. Science 273:749-750. return
10. Uno H, Tarara R, Else JG, Suleman MA, Sapolsky RM (1989): Hippocampal damage associated with prolonged and fatal stress in primates. J Neurosci 9:1705-1711. return
11. Sapolsky RM, Uno H, Rebert CS, Finch CE (1990): Hippocampal damage associated with prolonged glucocorticoid exposure in primates. J Neurosci 10:2897-2902. return
12. Woolley CS, Gould E, McEwen BS: Exposure to excess glucocorticoids alters dendritic morphology of adult hippocampal pyramidal neurons. Brain Res 1990; 531:225-231. return
13. Virgin CE, Taryn PTH, Packan DR, Tombaugh GC, Yang SH, Horner HC, Sapolsky RM (1991). Glucocorticoids inhibit glucose transport and glutamate uptake in hippocampal astrocytes: implications for glucocorticoid neurotoxicity. J Neurochem 57:1422-1428. return
14. McEwen BS, Conrad CD, Kuroda Y, Frankfurt M, Magarinos AM, McKittrick C (1997). Prevention of stress-induced morphological and cognitive consequences. Eur Neuropsychopharm 7:(suppl)3:S322-328. return
15. Smith MA, Makino S, Kvetnansky R, Post RM (1995). Stress and glucocorticoids affect the expression of brain-derived neurotrophic factor and neurotrophin-3 mRNA in the hippocampus. J Neurosci 15:1768-1777. return
16. Nibuya M, Morinobu S, Duman RS (1995). Regulation of BDNF and trkB mRNA in rat brain by chronic electroconvulsive seizure and antidepressant drug treatments. J Neurosci 15:7539-7547. return
17. Luine V, Villages M, Martinex C, McEwen BS (1994): Repeated stress causes reversible impairments of spatial memory performance. Brain Res 639:167-170. return
18. Bodnoff SR, Humphreys AG, Lehman JC, Diamond DM, Rose GM, Meaney MJ (1995): Enduring effects of chronic corticosterone treatment on spatial learning, synaptic plasticity, and hippocampal neuropathology in young and mid-aged rats. J Neurosci 15:61-69. return
19. Gould E, Tanapat P, McEwen BS, Flugge G, Fuchs E (1998) Proliferation of granule cell precursors in the dentate gyrus of adult monkeys is diminished by stress. PNAS 95:3168-3171. return
20. Sass KJ, Spencer DD, Kim JH, Westerveld M, Novelly RA, Lencz T (1990). Verbal memory impairment correlates with hippocampal pyramidal cell density. Neurology 40:1694-1697. return
21. Bremner JD, Scott TM, Delaney RC, Southwick SM, Mason JW, Johnson DR, Innis RB, McCarthy G, Charney DS (1993): Deficits in short-term memory in post-traumatic stress disorder. Am J Psychiatry 150:1015-1019. return
22. Bremner JD, Randall PR, Scott TM, Bronen RA, Delaney RC, Seibyl JP, Southwick SM, McCarthy G, Charney DS, Innis RB (1995): MRI-based measurement of hippocampal volume in posttraumatic stress disorder. Am J Psychiatry 152:973-981. return
23. Bremner JD, Randall PR, Capelli S, Scott T, McCarthy G, Charney DS (1995): Deficits in short-term memory in adult survivors of childhood abuse. Psych Res 59:97-107. return
24. Bremner JD, Randall P, Vermetten E, Staib L, Bronen RA, Mazure CM, Capelli S, McCarthy G, Innis RB, Charney DS (1997): MRI-based measurement of hippocampal volume in posttraumatic stress disorder related to childhood physical and sexual abuse: A preliminary report. Biol Psychiatry 41:23-32. return
25. Stein MB, Koverola C, Hanna C, Torchia MG, McClarty B (1997): Hippocampal volume in women victimized by childhood sexual abuse. Psychol Medicine 27:951-959. return
26. Gurvits TG, Shenton MR, Hokama H, Ohta H, Lasko NB, Gilberson MW, Orr SP, Kikinis R, Lolesz FA, McCarley RW, Pitman RK (1996): Magnetic resonance imaging study of hippocampal volume in chronic combat-related posttraumatic stress disorder. Biol Psychiatry 40:192-199. return
27. Bremner JD, Licinio J, Darnell A, Krystal JH, Owens M, Southwick SM, Nemeroff CB, Charney DS (1997): Elevated CSF corticotropin-releasing factor concentrations in posttraumatic stress disorder. Am J Psychiatry 154:624-629. return
28. Saigh PA, Mroweh M, Bremner JD (1997) Scholastic impairments among traumatized adolescents. Beh Res Ther 35:429-436. return
29. Morgan MA, LeDoux JE (1995): Differential contribution of dorsal and ventral medial prefrontal cortex to the acquisition and extinction of conditioned fear in rats. Behav Neurosci 109:681-688. return
30. Bremner JD, Krystal JH, Southwick SM, Charney DS (1995) Functional neuroanatomical correlates of the effects of stress on memory. J Trauma Stress 8:527-554. return
31. Bremner JD, Innis RB, Ng CK, Staib L, Duncan J, Bronen R, Zubal G, Rich D, Krystal JH, Dey H, Soufer R, Charney DS (1997): PET measurement of central metabolic correlates of yohimbine administration in posttraumatic stress disorder. Arch Gen Psychiatry 54:246-256. return
32. Bremner JD, Staib L, Kaloupek D, Southwick SM, Soufer R, Charney DS (1999): Positron emission tomographic (PET)-based measurement of cerebral blood flow correlates of traumatic reminders in Vietnam combat veterans with and without posttraumatic stress disorder. Biol Psychiatry (In press). return
created 3/3/99, reviewed 3/5/00; modified 3/7/99; end-date 3/7/02.
5 TASKS OF GRIEVING, LOSS, TRAUMA RECOVERY
When you are ready to accept the reality of the Grief, Loss, and/or Trauma, follow the next steps. This process is more circular than linear meaning there is no hard stop end to it. It is more about moving through the layers of the onion, one bit at a time.
- Name what has happened. Simply open to begin the process of grasping the enormity of the event in the mind.
- Notice where in the body you might be holding that reality. If you can’t notice where in the body it is held, then imagine where it might be held.
- Then, allow yourself to feel the Feelings of Grief, Loss, and/or Trauma as Sensations in the Body — Let them Move Through You But Don’t Identify with them. See, visualize and sense them as energy that you must move through verses be stuck in.
As you move through those feelings and images of loss, grief and/or trauma you then move toward the next step of recovery.
Remember to separate what you are experiencing from the deeper reality of who you are. In other words, don’t Be the grief, loss or trauma you are experiencing.
Remember you are much more than the energy, feelings or sensations moving through you!
If your hands, legs or any part of the body wants to move – allow it. Let the energy wave through you, mobilize and find completion.
- Consider What Could Manifest in place of the Gap of the Grief, Loss and/or Trauma. If a part of your psyche, body physiology, thought process is attached to or saturated with the energy of grief, loss or trauma – imagine what could possibly take the place of the negative energy. What positive and healthy future could manifest? Imagine how it might feel in your body, mind and soul.
Imagine how your body might move and your thoughts and energy reorganize.
- Reinvest in Life – Readjust to the Environment without the Grief, Loss, and/or Trauma. Find yourself again and be the new you in the world. Emerge from the Cocoon! Completion of the metaphorical death – rebirth process and discover who you are now.
- Anchor Into Your Core Being, not your ego-based false self – The old patterns and ways of thinking and acting may return, just don’t attach to them. Instead, anchor into your true self. It is the dimension deeper than the false self. It is the dimension of your deeper god-self that was never traumatized or hurt.
Imagine, feel, sense your Core Being strengthen and the old melt away. From the place of Core Being you can feel your imperfections and defenses, you just don’t attach to them and think they are the truth of who you are.
Eventually you will be able to more often return to Core Being and take action and be in relationship from this place.
My definition of enlightenment is:
(1) knowing, feeling and anchoring into this deeper true self within us and
(2) when we get triggered out of this place, being able to return quicker and quicker (even if it takes a few days) back to our CoreBeing.
Core Being is a deeper dimension from the false self that gets programmed within us. It is our unique and whole true essence that is expressed even before conception and birth.
Grief, Loss and/or Trauma changes us. As we emerge from them, we are forever different. From difficulty the riches can be found. Find the gift in every moment. Find your internal riches of the deeper truth of who you are. Emerge!
Feel free to reprint as long as credit is given to: Carolyn Eberle, MA, LPC; Founder, 720/530-7621
TRAUMA TO DO’s and DON’TS
Patience – going slow
Catharsis in not Healing- simply because you feel an emotion does not necessarily heal the emotion.
You must have a sense of your deeper true self and look at the trauma and the emotional pain as energy moving through you and not the truth of you.
Don’t Over Identify with the Trauma. Be the Light you are and anchor into your true self.
If you connect to trauma with dense consciousness/energy – you get more trauma.
Access – don’t charge trauma. Bring in higher vibrational energy, positive belief systems, and good sensations in the body.
You must have an empowered witness or observer in order to re-pattern verses re-experience trauma.
Strongly Positively Resource a Client or Yourself Before going into Trauma
You heal trauma by brining in the positive belief system and true sense of self.
If you don’t feel positive sensations in the body afterward, chances are you have re-traumatized and/or disassociated
Deep trauma work necessitates the ability to hold two places at one time. One place in the trauma and one place connected to your core, divine truth.
Replaying trauma tends to rewound and re-traumatize so if you replay it, make sure there is a positive shift toward re-scripting the past. Let your mind, energy, body (ME-B) systems find a positive outcome and let your body move in a manner that mirrors that positive outcome.
If you or your client thinks they are the pain, then they create a deeper grove in the unhealthy “train track” instead of creating a bridge to a healthy “train track” — subsequent healing becomes more difficult because the body is programmed to respond in a misaligned manner to the external world- Hyper or Hypo sensitivity. Lower brain functions take over and cognitive choice is removed.
Trauma is in the ME-B systems – the physiology of the body, brain chemistry, nervous and energy must re-patterned for optimum healing to take place. Learn how to do this in all ME-B systems.
Less is usually more – because trauma happens in accelerated time, you must let each part integrate before you do more. I call it accessing the trauma, NOT charging it. This way you can reprogram the ME-B system.
If you reprint, please give credit to Carolyn Eberle, MA, LPC, Mind Energy Body Institute; www.mindenergybodyinstitute.com; 720/530-7621.
http://www.myshrink.com/counseling-theory.php?t_id=85
Freeze Response
![]()
Dr. Suzanne LaCombe, April 4, 2007.
Updated: January 6, 2010.
Ever catch yourself holding your breath, or spontaneously heaving a deep, long sigh? Read on as I propose an intriguing possibility for why this happens. (The answer is found in our mammalian wiring!)
Many people are aware that as mammals we’re wired for fight or flight. This automatic reaction propells us into action during times of danger. However, few are aware that the freeze response is an equally important and related survival mechanism.
If you enjoy nature shows (no, not March of the Penguins!) you’ve probably already seen the freeze response. You’ve also seen that a predator will ordinarily ignore prey that is not moving, for fear of contracting disease.
In the last moments of the chase, when there is literally no possibility of "fight or flight", the victim will experience the freeze response. It will feign death by "playing possum".
The freeze response is hard-wired in our reptilian brain. When "fight or flight" is not an option, our autonomic nervous system goes into a freeze response and we become immobilized.
The phrases "scared stiff" or "frozen with fear" reflect this mammalian characteristic. A deer that’s "frozen in the headlights" is responding likewise.
What’s important to understand.
The freeze response is an automatic, non-conscious reaction that occurs when mammals face an overwhelming threat. This response is a last ditch effort to save itself. In some instances it is the optimal survival tactic.

Where’s the ‘ol fight – flight’ when you need it!
Many who seek counseling for relief from the symptoms of trauma are puzzled when they recall how they froze in the face of inescapable danger. Indeed, they are frequently filled with shame about their reaction to what happened.
Our survival instinct is extremely strong. It is not easily overridden by the neocortex (i.e. our intentional self). In the same way that you cannot tell yourself to have a good night sleep, you cannot tell yourself not to freeze. The body chooses. It’s the optimal response at the time.
The Freeze Response
There is a growing awareness by neuroscientists that our evolutionary heritage has a greater impact on the nervous system than was previously thought. These new theories promise exciting new possiblitlies for improved human health and well-being.
This new perspective suggests that "freezing" doesn’t refer just to being motionless. It also refers to how the nervous system manages arousal during moments of traumatic stress. It is this type of freezing that causes many of us to develop trauma symptoms long after the danger has passed. In other words we may go into freeze yet not be aware of it.
Let me explain.
During an traumatic event an enormous amount of energy is released by our neuroendocrine system. This enables us to fight or flee. However, fight or flight is not always an optimal strategy in modern life.
For example, if my boss infuriates me I don’t really want to punch his lights out (i.e. fight). If my car is about to collide with another there is usually little advantage to jumping out of the car (ie. flight)–even if I had time to do so.
However, if there is sufficient resiliency in your nervous system you will be able to discharge this energy without being traumatized. For many people however this life-threatening experience sets the stage for dysregulation. The energy mobilized by the perceived threat gets "locked" into the nervous system when we go into freeze.
In these situations you may not even realize that you went into freeze, yet several months later you can still be reeling from the effects of an accident. One theory is that the nervous system has not yet discharged the energy that was mobilized for fight or flight.
This freeze response sometimes reveals itself when you breathe. Holding your breath and shallow breathing are both forms of freeze. The occasional deep sigh is the nervous system catching up on it’s oxygen intake.
Implications for counseling
What’s even more intriguing is the theoretical possibility of preventing post-traumatic symptoms. It appears that the more the nervous system is dysregulated, the greater is the tendency to move into freeze. (See Runnin Scared below)
I find this exciting because I look forward to a time when keeping our nervous system regulated is as common as dental hygiene.
Equally exciting are the implications for somatic therapy. As our clinical practices1 show, integrating the body into psychotherapy tends to restore resiliency to the nervous system, a key factor in its efficient regulation.
RELATED TOPICS
Runnin Scared: This is your brain on 9/11.
Scared to Death![]()
Regulation
You may find the discussion in the Counseling Psych Cafe helpful as a couple members describe the process of coming out of freeze.
Notes
1. I understand that this outcome is more easily identified in body-oriented psychotherapy. Since few clinical trials have been conducted so far, this observation remains outside mainstream psychological practice.
Resiliency may well be a common outcome in other psychotherapies however as I understand it, resiliency is not often tracked. That is, it isn’t noticed because therapists aren’t looking for it. Body psychotherapists are trained to look for it.
References
Levine, Peter, A. (1997). Waking the Tiger: Healing Trauma. Berkeley, California: North Atlantic Books.
Porges, Stephen, (1995). Orienting in a defensive world: Mammalian modification of our eveolutionary heritage. A polyvagal theory. Psychophysiology, 32, 301-318.
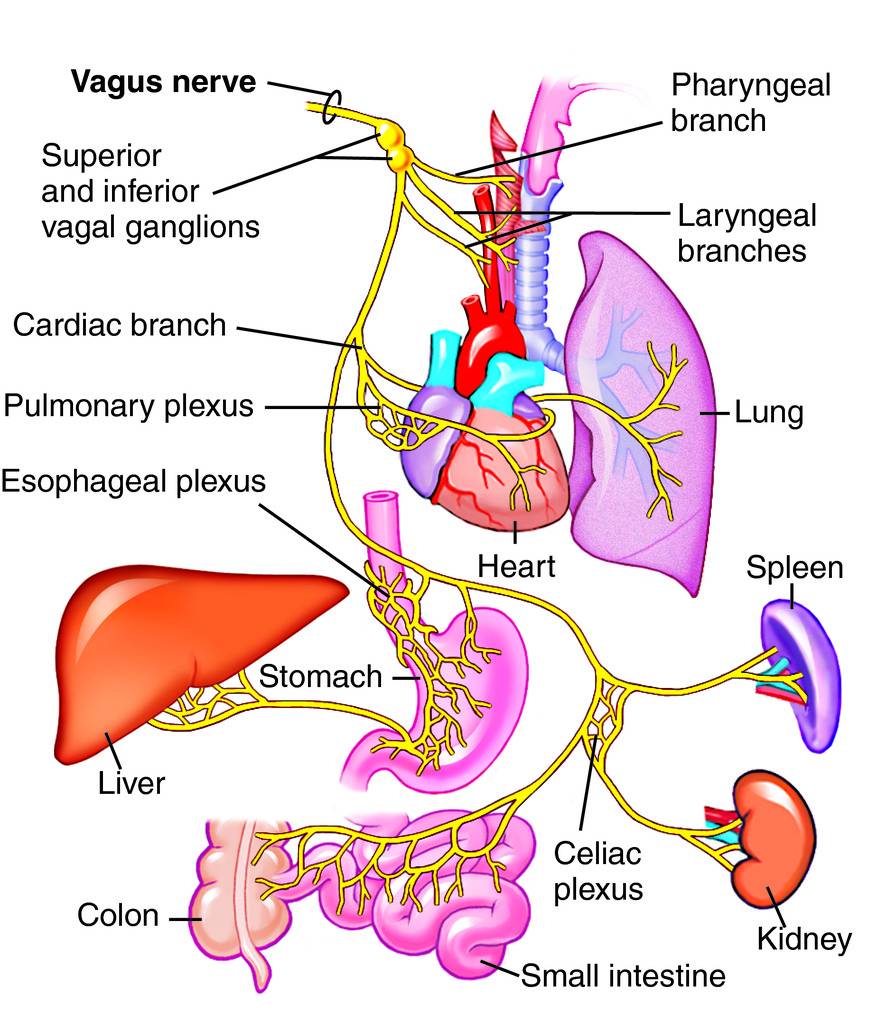
Stephen Porges’ identified two, not one, branch of the parasympathetic nervous system. His discovery of the dorsal vagal (and its relationship to the ventral vagal) has helped us to understand the relationship of the freeze response in the development of PTSD. The polyvagal theory has also been useful in understanding the mind body connection. You can access his classic 1995 article here (you will be taken off site:
Orienting in a Defensive World…A Polyvagal Theory.
Rothschild, Babette, (2000) The Body Remembers: The Psychophysiology of Trauma and Trauma Treatment, London: W. W. Norton & Company.
Scaer, Robert C., "Precarious Present" in Psychotherapy Networker, Nov/Dec 2006.
Scaer, Robert, C., (2005). The Trauma Spectrum, New York: W. W. Norton & Company.
Scaer, Robert C., (2001) The Body Bears the Burden, Haworth Press.
External Links
Here’s a more comprehensive look at the freeze response. These researchers differentiate the initial "stop, look, listen" type of freeze that happens when mammals first encounter danger from the "tonic immobility" or "fright" response that happens when there is no option for fight or flight.
Does Flight or Fight Need Updating?